Failing to Scale: Fixing Common Missteps in mHealth Ventures
Telemedicine and mHealth systems have the potential to improve the efficiency, accessibility and reliability of fledgling health care systems in developing countries. By now the image of the rural, low-income individual receiving a virtual checkup from a remote doctor through a computer screen, phone or tablet has become commonplace – at least in marketing materials or slide decks. Alongside telemedicine systems like these, the rapid proliferation of smartphones in developing countries has enabled mHealth systems that connect new moms to educational resources to care for their infants or apps that improve drug adherence for tuberculosis and other diseases.
However, the vast majority of these ventures experience pilotitis – the inability to survive beyond the pilot phase. To understand the causes of pilotitis, our team with undergraduate students in the Humanitarian Engineering and Social Entrepreneurship (HESE) Program at Penn State studied 35 relevant telemedicine and mHealth projects and categorized recurring failure modes. We found that risk factors for pilotitis fall under six core failure modes: financial challenges, technological challenges, employee management, customer interactions, organizational relationships and contextual challenges (Figure 1).
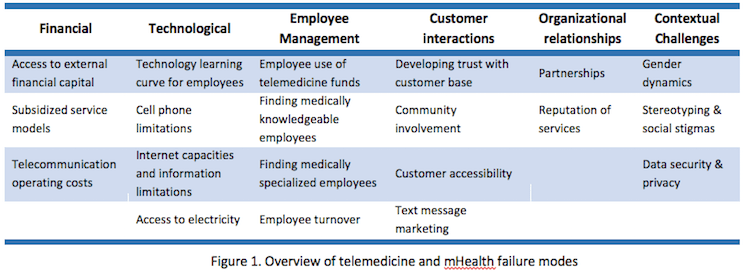
1. Financial Challenges in telemedicine
Startup capital and a sound revenue model play a pivotal role in sustaining a telemedicine system beyond its initial pilot. When telemedicine systems have their origins outside of the country of operation, as is often the case, the operating costs and overheads are even higher. Access to external capital from government grants, donor funds or private equity is important in the early stages of operations when demand is low, the technology is still being tested and the number of people well-versed in the use of the system is limited. Offering a free-of-charge service can quickly grow the customer base and scale the venture, but eventually, a financially sustainable revenue model needs to be established. Several telemedicine ventures provide free services but are dependent on donations from wealthier nations. Shifting from cost-free services to paid services presents several risk factors when consumers are not accustomed to paying for (normally free or subsidized) health services. Operational expenses can increase exponentially as the user base grows. While text messaging is often inexpensive, a mass text message sent to 10,000 users can get expensive.
2. Technological Challenges for mhealth ventures
Almost 90 percent of the world population (above the age of six) has a mobile phone. Many health ventures have attempted to use these mobile devices as the primary method of data collection and communication. In spite of the rapid growth and accessibility of telecommunication technologies, many hurdles remain. Improving the technological literacy of employees can help shorten and accelerate the technology learning curve necessary to operate and sustain projects. Training is most effective when implemented with context-specific linguistic and gender norms. While smartphones are becoming increasingly common and internet costs are coming down, most cell phones used in the developing world are simple handsets with limited computing power, low memory and restricted text messaging. Ventures often use the pilot phase to gauge the amount of data/storage needed, or to develop store-and-forward mechanisms that send data to a central server as soon as the user reaches an area with adequate cellular service to ensure secure and robust data backup. Cell phones and other battery-operated devices like automated blood pressure cuffs and blood glucose monitors need to be charged on a regular basis; the inability to charge devices can severely impact customer sentiment. Although solar chargers are becoming widespread, other alternative modes of charging that are convenient, reliable and inexpensive need to be identified.
3. mhealth success requires effective employees
Due to the sensitive nature of certain health conditions, such as HIV or mental health issues, hiring trustworthy, disciplined and professional employees is essential. We found that individuals acting in self-interest or lacking business acumen often make business decisions and seldom take a long-term view by, for example, reinvesting revenues into the project. Further, brain drain makes it difficult to find medically knowledgeable employees with sharp business skills, which leads to task-shifting to community health workers (CHWs). While CHWs can be excellent champions for addressing last-mile health care challenges, they have limited training to make clinical decisions, and their community connections make it difficult for money to change hands. Venture employees must also be specialized in their field of care (e.g., pediatrics, optometry, internal medicine), especially if the project wants to target a specific health issue. In cases where qualified employees are scarce but demand is high, a referral system may be possible using local health workers, with those in greatest need contacting the medical professionals directly or traveling to a separate facility. High rates of employee turnover are also a daunting concern for early-stage ventures that have invested resources to train employees who later leave to pursue more lucrative opportunities.
4. improving Customer Interactions in telemedicine
For telemedicine and mHealth ventures to cement their trust and credibility, they must have regular, positive, high-quality interactions with their customers. Such interactions can include sending weekly text messages to patients, engaging the community through various health events or using a face-to-face advertising model in lieu of print media so as to rally communities to become actively involved in improving their health. By integrating themselves into communities, telemedicine ventures can both increase the customer base and build a better brand name. While improving accessibility fosters strong customer interactions, poor networks and physical availability can compromise the brand perception. Many telemedicine systems rely on text messaging to deliver information to their customers efficiently. Consistent messages that are well-aligned with the venture’s brand can help grow the customer base while establishing trust and credibility. For instance, attaching a small brand logo at the end of each text message helps enhance reputation.
5. The value of Organizational Relationships
To create a sustainable and scalable venture, telemedicine and mHealth initiatives must build and leverage relationships with other organizations including nonprofits, universities or government agencies. Ventures need to discuss the equity of work, finances and time that each partner will contribute – and what they expect in return. A primary strategic goal, a shared definition of success and a plan to scale ensure that all partners are working toward the same vision. Nonetheless, partnerships are just one element of organizational relationships; the reputation of a venture largely dictates its success. If services are unreliable, low quality and/or not aligned with local values, then telemedicine ventures seldom grow beyond the pilot phase. A public relations campaign that brings high-ranking officials and local opinion leaders together to vouch for the project and be the first paying customers can enhance its reputation and credibility and pave the way for paid services.
6. Contextual Challenges in mhealth
Telemedicine projects have to deal with their own geography-specific gender inequities related to varying education levels, access to phones, role in family and community health, and access to resources needed to patronize – as well as offer – telemedicine services. In some areas, female health workers may be chided and the social status of their family could be threatened for their involvement in family planning, interactions with men and their travels across villages. Stigma around mental illness and HIV/AIDS may prevent individuals from seeking health care. In addition to providing health services, telemedicine initiatives should devote resources toward changing cultural views through community outreach and education efforts. If a telemedicine system wants to collect and track health information, especially on mobile devices, the data should be stored in a safe and legal manner, and shared only with customer approval and after a thorough analysis of the desired and potential implications. Employment legality is another factor that affects health worker recruitment. Potential health workers may be discouraged from accepting a position due to their unfamiliarity with, or skepticism of, the legal obligations surrounding employment with a telemedicine venture. Rather than using a series of contracts, one solution for telemedicine systems is to use incentives to ensure that their employees are being responsible and professional.
In summary, the largest barriers to the viability of telemedicine ventures are related to the social, economic and legal context of operation. While new affordable technologies that simplify and streamline processes can accelerate the growth of telemedicine ventures, a deeper understanding of the context and the presence of strong value propositions can help design stronger business models that are able to scale beyond the pilot phase and realize their full potential. The second part of this series will review the value propositions of telemedicine systems.
This blog is a summary of a research article: Sundin, P., Callan, J., Mehta, K., “Why do Entrepreneurial mHealth Ventures in the Developing World Fail to Scale?” Journal of Medical Engineering & Technology, Vol. 40, No. 7-8, pp 444-457, 2016)
Khanjan Mehta is the vice provost for creative inquiry and director of the mountaintop initiative at Lehigh University.
Photo by Intel Free Press via Flickr
- Categories
- Health Care, Technology