The Universal Clinic: A New Paradigm for Rural Health Care?
Advances in medicine over the past 100 years have made it possible to prevent, diagnose and treat most common conditions responsible for sickness and death. But an unacceptable number of people, mostly women, infants and children, continue to suffer or die untreated, from conditions that are avoidable and treatable. These statistics are concentrated in developing regions, especially in rural areas, where systemic gaps in financial, human and infrastructure resources lead to yawning gaps in health care delivery. There is an acute shortage of clinics equipped to deliver meaningful – if any – health care and women and children, the most vulnerable constituencies, are hardest hit.
These systemic gaps will take a while to bridge organically. Which begs the question: Until this happens, can new technology-enabled solutions make it easier to provide universal health care? And if this is possible, why hasn’t it happened yet?
Market-driven solutions have not emerged because private providers in rural areas are too small and fragmented; their lean pockets have not warranted sufficient attention from traditional technology companies. Governments and donors, on the other hand, have focused on narrow issues, disease verticals and incumbent delivery models. The mandate for investing in a step change to health care delivery systems has thus been limited.
Universal Clinics, an initiative at the Institute for Transformative Technologies (ITT), is committed to solving this problem. We are building the Universal Clinic, a cohesive platform of integrated technologies to operationalize clinics in resource-constrained settings with high-quality primary and maternal health care in a cost-effective and scalable manner, using a “hub-spoke” model for health care delivery.
The Universal Clinic is comprised of four modules. The core module has a digital platform for patient information management and distributed delivery of comprehensive services across large networks of rural clinics, e.g., remote consultations with doctors via telemedicine, clinical decision support tools for rural clinicians, referrals and escalation of cases, etc. Clinical applications on this platform are integrated with point-of-care diagnostic devices to enable accurate and timely diagnosis and treatment supported by rich clinical data collected during patient consultation. This module allows clinics to be deployed with a hub-spoke model where expansive networks of rural clinics (spokes) can efficiently leverage the capabilities of a remote hospital (hub).
The second module is equipped with therapeutic devices, e.g., post-partum hemorrhage kits and neonate resuscitators for safe deliveries; the third has utility equipment to run clinics; and the fourth is a durable, easy-to-set-up structure for housing clinics.
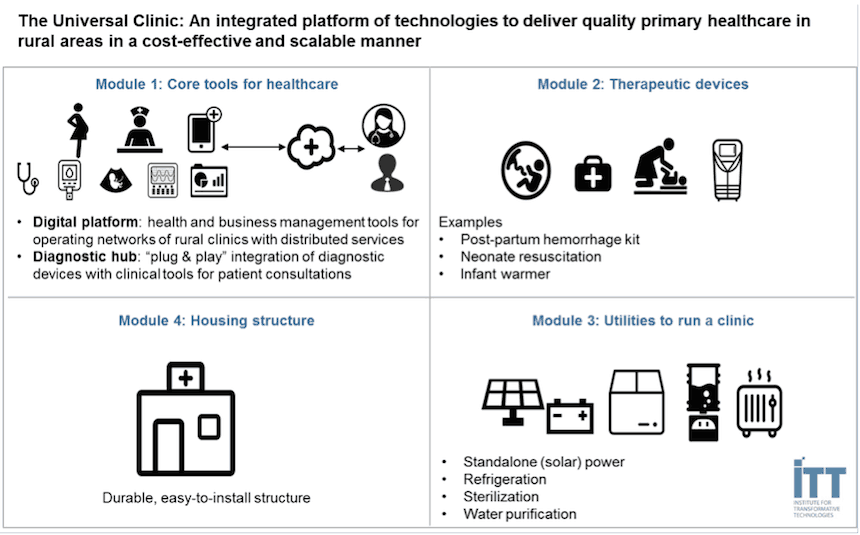
The Universal Clinic can be deployed as a turnkey solution or in a modular fashion, e.g., existing under-resourced clinics can be outfitted with one or more of these modules to deliver better services. When deployed with the hub-spoke model, expansive networks of rural clinics can leverage the capacity of remote hospitals to deliver services.
There are many one-off technologies but no sustainable delivery model for rural health care that can absorb these technologies. Our intent is not to reinvent the wheel, but to funnel, optimize and integrate best-of-breed technologies into a cohesive plug-and-play platform for a new paradigm of health care delivery – to provide quality services cost-effectively and at scale in rural markets. Health care providers across the board – public, private and NGO-led – face numerous and multifaceted challenges when it comes to providing meaningful health care in rural areas. Here’s how the Universal Clinic addresses the key challenges:
Quality
Vertical interventions like immunizations and screening for specific conditions are necessary but not sufficient for good health care. The ability to restore the health of a sick patient by diagnosing and treating a range of common ailments is the cornerstone of meaningful health care. This requires medical expertise and patient health information, but both are acutely limited in rural settings in developing regions. There are roughly 30 doctors on average for every 10,000 people in OECD countries; in most sub-Saharan countries the number is one or two (per 10,000 people) and most of these doctors operate in urban areas, according to the World Health Organization (WHO).
Rural clinics have limited diagnostic capabilities due to lack of affordable and appropriate devices, lack of trained technicians, lack of power, etc. Patients are thus misdiagnosed (and mistreated) or referred to advanced (and remote) facilities, an extra trip involving cost and time that patients can ill afford and thus often skip, leading to follow-up losses. Well-equipped facilities are sparse, overloaded and have long wait times and poor customer service. Lack of patient history also undermines quality of care. Patient information is typically recorded manually on paper (if at all), making it slow and costly to manage and share – plus it’s often erroneous. To make matters worse, patients often lack reliable means of identification, e.g., an ID card or driving license. Finally, tools to help clinicians follow standard protocols for quality care and to enforce adherence by clinicians are limited.
The Universal Clinic will come with tools to register patients and maintain rich patient history, e.g., health data, symptoms, prescriptions, referrals, etc., using biometric identification, significantly improving accuracy and speed of care and making it possible to hold both clinicians and doctors more accountable for health outcomes. This has far-reaching implications for the larger health system. As more cases are effectively diagnosed and treated at primary care clinics it will pre-empt needless escalation to advanced facilities, easing the pressure on an already overburdened patient population and health care delivery system.
In most rural areas today, a pregnant woman arriving at her local health center lacks access to a trained doctor and essential diagnostic capabilities, resulting in critical delays in appropriate treatment. The Universal Clinic will change all of this. A tablet-powered tool – deployed over the Universal Clinic’s digital platform – will instruct the clinician on appropriate tests and protocols for care and a doctor will be available over tele-consultation to interpret results and advise the clinician. Point-of-care tests for protein in urine combined with blood pressure, edema and blood sugar will help the clinician diagnose and treat the woman for pre-eclampsia, a driver of maternal morbidity. A rapid hemoglobin test will determine whether she is severely anemic. A blood type test will confirm an appropriate donor source for blood transfusions during delivery and mitigate the risk of post-partum hemorrhage, another driver of maternal morbidity. A rapid HIV test will ensure that certain infections are not overlooked. If she is running a fever, a suite of rapid diagnostic tests will detect life-threatening infectious diseases such as malaria, dengue, typhoid or common urinary tract infections through comprehensive urinalysis. Blood pressure and pulse oximetry will determine quickly whether fluids or oxygen are required for stabilization. All of this will take place without her leaving her village. Her medical history will be stored, tracked and managed meaningfully to ensure that she (and her child) continue receiving quality and accountable care.
Financial sustainability
Health is a human right and a public good and one may argue that a focus on financial sustainability is therefore misplaced. But the hard fact is that financial resources, both public and private, fall drastically short of what is needed for universal coverage in developing regions. According to WHO, the average annual health care expenditure in OECD countries is over $5,000 per person; in sub-Saharan Africa and South Asia it is less than $100. Innovative low-cost models are emerging but are mostly limited to urban and peri-urban areas as their economics cannot sustain the dynamics of the rural market, featuring very low, unpredictable and seasonally fluctuating incomes and a nascent market where health-seeking behavior and willingness to pay is not yet fully understood. Making rural health care cost-effective is a critical lever for universal coverage; it will attract private providers to rural markets and enable public and NGO-led systems to do more with less.
The Universal Clinic offers important benefits for financial sustainability. The two big cost drivers for a clinic are capital costs – the one-time cost for setting up a physical clinic – and ongoing salaries for doctors. Currently it costs $100,000 to $200,000 to set up a full-fledged outpatient clinic (using market benchmarking of full-fledged clinics for primary and maternal care – outpatient services – in Kenya). The Universal Clinic leverages low-cost innovative devices and equipment and standardized design and assembly to lower upfront costs. Further, telemedicine enables cost-effective remote utilization of doctors. Diagnostics at the clinic save patients trips to other facilities, significantly reducing follow-up losses and the effective cost of treatment. Both clinics and patients can enjoy economic benefits from these.
Traditional clinics lack digital information systems and tools making it costly and hard to administer health financing services and to streamline business operations. With the Universal Clinic’s digital platform, such services can be deployed seamlessly across large health care networks with economies of scale and scope. An important issue that is not fully appreciated is that poor quality of care and customer service diminishes demand for health care in a market where it is weak to begin with. The benefits of the Universal Clinic areas can improve sustainability by boosting demand for health care.
Scalability
Physical barriers are a key limitation to scaling coverage in rural areas. Electricity is essential for health care services but more than 80 percent of the global population living without electricity are in rural sub-Saharan Africa and developing Asia. Setting up a standard clinic is also a multifaceted problem; supply chains are highly fragmented and often unreliable, skilled labor is scarce and providers lack standardized tools for setting up clinics.
We believe the Universal Clinic makes it possible to scale care to resource-constrained tracts. A stand-alone power management system makes it possible to serve off-grid areas. The Universal Clinic’s flavor of telemedicine and its suite of medical devices have features to operate robustly in low-bandwidth and energy-constrained settings. Finally, it offers the ability to assemble and operationalize quality clinics in a standardized fashion, making it easier and faster to build new clinics and upgrade existing ones.
The Sanskrit word for the healthy is swa-astha, or one who is self-reliant. But good health as the cornerstone of self-reliance eludes millions of low-income rural people in developing regions. By enabling health care systems to provide expansive coverage of affordable, high-quality and scalable health care in rural areas with the Universal Clinic, we hope to bring one of the most pressing issues in development and resilience to a tipping point within the span of our lifetimes.
Subarna Mitra is vice president, Access to Healthcare, and one of the founding members of the Institute for Transformative Technologies.
Note: Dr. Shashi Buluswar, CEO of ITT, Urvashi Gulia, ITT’s communications director, and Dr. Anna Stratis, medical adviser, also contributed to this post.
Photos courtesy of ITT
- Categories
- Health Care



