The Digital Revolution in Healthcare: How COVID-19 Has Accelerated Efforts to Close the Health Data Gap in Emerging Markets
In many countries, there is a significant lack of accountable, accurate, real-time health information, on key topics ranging from the prevalence and incidence of disease to the current supplies of medication and equipment. This data gap impacts every stakeholder in the healthcare ecosystem, most notably patients and providers. With most medical information stored either on paper or on unconnected and often incompatible digital platforms, health statistics are largely disjointed, incomplete and inaccurate. That means key health information, such as the percentage of the population with heart disease, is unknown in many emerging markets. Yet this data is integral to determining where to focus healthcare spending and medical resources – e.g., how much medication, supplies and equipment to procure, how to price insurance policies, and where to focus staffing and other resources.
Addressing this data gap is especially important, as healthcare is one of the most significant expenditures across countries as a percentage of GDP, especially in emerging markets. And, unlike other industries, a more effective, compliant and resilient healthcare system provides the opportunity to reduce costs and save money – billions of dollars that can be routed elsewhere, benefitting all stakeholders and citizens. But without accurate health information, it is impossible to build a resilient health system that minimizes the cost and maximizes the quality of care for patients.
However, there’s reason to believe that this situation is changing: COVID-19 has highlighted the importance of better health data, and improvements are already underway in many countries in response to the pandemic. Below, I’ll discuss how healthcare systems in emerging markets are navigating the transition to digital data solutions, and how COVID-19 has both accelerated these efforts and highlighted some of their key challenges.
From Paper to Digital: The Evolution of Health Data in Emerging Markets
When you visit health systems in emerging markets and see their clinical care up close, one of the first things you notice is the amount of paper. Rooms may be filled from floor to ceiling with old medical records. Even if the facility uses an organized medical record or health information system, paper is still prevalent, commonly used for recording key information and reports, and to give patients everything from prescriptions to vaccine cards. If a patient goes to another facility, their paper-based medical records do not come with them – and even if two facilities use the same digital record-keeping system, they usually don’t communicate. This prevents physicians and health workers from accessing accurate, critical patient information, impacting both the cost and quality of care and their ability to manage their resources. With many of these health systems already constrained due to physician shortages, these inefficiencies further compromise their ability to provide effective care, leading to wasted resources, unnecessary tests and longer appointment times that reduce the number of patients who can be seen each day.
However, even when healthcare providers attempt to move beyond these paper-based information systems, their efforts are often hampered by several key issues:
- Physicians and the broader health industry are often late adopters when it comes to new processes and technologies.
- Tech solutions are often primarily focused on billing and statistics, and not on the clinical needs of physicians or hospitals, which can make these tools less intuitive. Even in the U.S., many physicians are not happy with their electronic medical record platforms and find them confusing or not user-friendly.
- There is minimal interoperability between digital health systems. Even if two clinics in the same health organization are using the same system, they often cannot aggregate information or pass medical records easily across facilities.
- Many health systems lack the necessary infrastructure and equipment to successfully use a digital platform, including both computers or tablets and consistent internet connectivity.
The lack of interoperability is an especially critical point. Many grants are given each year to tackle specific health issues like malaria or tuberculosis, often funded by the same organizations. Despite that, each project captures their key data points in their own way, preventing easy, insightful analysis of the aggregated information they’re generating. An interoperable network or single platform would address this issue while also freeing up more funding for other projects, since these grants often include signficant funding intended to cover technical costs that would be redundant if there was a unified system.
The Impact of the Lack of Digital Health Systems in Africa
I spent over three years living in Kenya and Cote d’Ivoire, meeting with key stakeholders, getting feedback and creating my company, PocketPatientMD, which offers a customizable and interoperable digital health data platform in multiple languages. I’ve also had the opportunity to travel and do independent research on health systems in countries across Asia, Africa and Europe. I encountered these data challenges in almost every place I visited, but I experienced them most extensively in Africa. While living on the continent, I met with healthcare stakeholders at all levels – including doctors, Ministries of Health, First Ladies, public and private organizations, and others – to explore how our platform can address their health data problems.
While sub-Saharan Africa accounts for roughly 11% of the global population, it accounts for over 24% of the global disease burden, and there is very little real-time health information available across the continent. In my time there, I saw how this leads to shortages of medication and equipment, and how it impacts the ability of insurance to help these populations. The region has had examples of successful data-sharing systems, such as those for contact tracing used during Ebola outbreaks, which effectively enabled neighboring countries to work together to understand and control outbreaks. But these examples are the rare exception.
My work on the continent also gave me a first-hand view of a key driver of the health data gap: the fact that frontline health workers and doctors are the most affected but the least involved in many key decisions which impact clinical care. Decisions about workflow, platforms and systems are often made by outside parties with a focus on administrative and business functions, and so they often lack an emphasis on the patient-doctor relationship and clinical experience. Even when a health system has access to efficient digital data solutions, these solutions often fail to meet the needs and demands of each stakeholder – beginning with the provider – due to issues such as lack of administrative approval or connectivity, the cost of data, or confusion over how to use the solution properly to meet specific clinical needs. A lot more can be accomplished with a lot less if these providers – the physicians and frontline health workers – have their needs addressed. This will require leading stakeholders – from Ministries of Health to hospital networks and health systems – to listen to the needs of physicians, giving doctors the power to provide feedback about which tools meet their needs and objectives, and what systems they want to use every day.
How COVID-19 Has Highlighted the Need for Digital Health Solutions
On the positive side, COVID-19 has highlighted the need for change. Pandemic-fueled reductions in non-essential care and closures of offices have led to a significant increase in the use of, and need for, telemedicine tools. Doctors who once were resistant to going digital are now seeing patients remotely via mobile platforms – and this provides them with more of a reason to use digital solutions and move away from paper, which is a key behavioral shift and first step. This shift can be seen in other provider behaviors: In February 2020 it could be difficult to get five physicians onto a call together, but by August, webinars with over 50 doctors could be held seamlessly. This is a huge step in the right direction.
COVID-19 has also highlighted the need for organized contact tracing and disease tracking, illustrating the importance of accessing information in real-time. I saw this myself in my work with PocketPatientMD. One country we work in had a very high COVID-19 morbidity and mortality rate, yet doctors there were only able to track and monitor the sickest patients. Within about a month of using our platform, one doctor we worked with was able to follow-up with more people, resulting in an improvement of 50% in morbidity and mortality. The platform was also used to control a COVID outbreak via contact tracing in Asia, all with remote training and demos.
But though the pandemic may have unlocked the first obstacle to digital health in highlighting the value of moving on from paper, other challenges remain, and more progress is needed. It is important to continue to push forward with innovation and digitization so we can respond, recover and rebuild faster from the current crisis, while preparing for future health needs.
We have seen these challenges firsthand with PocketPatientMD. We are providing our platform at no cost to healthcare providers or organizations, with our revenue coming from pharmaceutical firms, device manufacturers and insurers who support the platform to help increase access to care, reduce waste and better allocate resources to maximize impact. We have received high-level approvals for pilots from several organizations and Ministries of Health. Yet these approvals – and the benefit of being a free platform – are not enough. Physicians and many facilities, especially public hospitals and clinics, need electronic equipment (i.e., computers or tablets) to utilize our services, and the cost of data can also be significant. Subsidies for data access and equipment purchases – via government, private investors, partnerships or even donations – can address these barriers and help increase uptake. Subsidies could also be employed to incentivize doctors and give them benefits for digitizing, which could have benefits not only for providers and health systems, but for the entire population.
One of the final challenges facing digital health data initiatives involves data security and ownership. There are various existing measures to improve security and mitigate risks, such as anonymizing information and adhering to U.S. and European (HIPAA and GDPR) guidelines and international standards. Unfortunately, many emerging countries are unable to meet these guidelines, since their data rules are still being finalized and their data security may still be lacking. Additionally, with many health data platforms the users do not own their own data, and some platforms may be designed to either acquire data indiscriminately or chase statistics about specific health conditions for research purposes, instead of only obtaining the data they need to meet the needs of their actual users. This is something we work hard to address at PocketPatientMD, but it’s nevertheless a concern many doctors have. To avoid this issue, our data-gathering efforts focus on the entire clinical picture and physician-patient relationship, aiming to build a solution that operates within that scope so everyone can benefit.
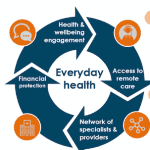
One of the big lessons of COVID-19 is the importance of resilient, responsive healthcare systems that can understand and respond to trends and events in real time. And the key to building those systems is ensuring that key stakeholders – physicians and frontline health workers, Ministries of Health, pharmaceutical firms, device manufacturers, insurers, and others – have access to accurate, real-time data. The pandemic has given us a chance to see health systems at their breaking point. If we address their data needs and give doctors the digital tools they want and need, we can ensure that every stakeholder in every health system benefits from the digitization of healthcare, providing the best care possible to each person – both during and after the current crisis.
Mark Wien is Founder and CEO of PocketPatientMD.
Photo courtesy of Ami Vitale / World Bank
- Categories
- Coronavirus, Health Care