Nine Ways to Make Money in mHealth: The Top Value Propositions from a Study of 234 Projects in Emerging Markets
As discussed in part one of this blog series, the majority of telemedicine and mHealth initiatives fail to survive beyond the pilot stage. Many telemedicine and mHealth projects owe their genesis to research grants focused on the clinical outcomes of the intervention. Researchers seldom give thought to, or have an interest and expertise in, developing sustainable business models. Alongside focusing on the macro clinical outcomes, identifying, articulating and validating value propositions for customers can help develop viable business models.
While a researcher may design an intervention to reduce the spread of infectious disease, a customer would be interested in preserving their (and their family’s) health and not miss days at work. This simple shift of placing customers at the core of the venture, understanding their context, challenges and choices, and solving a deeply-felt problem that they are willing to pay to remedy is the holy grail of sustainable long-term operations. My team studied 234 mHealth projects in developing countries and developed a typology of the nine most common value propositions, which are presented below.
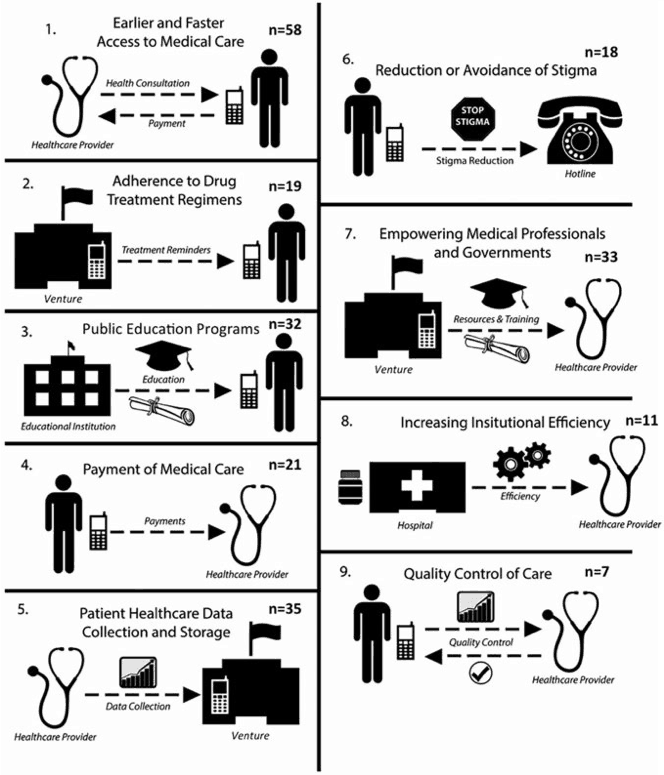
Figure 1. Typology of value propositions of telemedicine and mHealth ventures.
1. Earlier and faster access to medical care
Projects can bypass long and costly travel to clinics or hospitals by replacing face-to-face appointments with one of three approaches: 1) doctor hotlines where individuals call for medical advice; 2) local nurses, trained community health workers, or clinical officers who collect and send health information from patients to physicians via phone call, video conference, text messages or other media; or 3) self-screening technologies aided by phone, websites or other media. The target audience includes expectant mothers, children, women, and individuals with specific conditions such as HIV, tuberculosis, or skin complications. Such ventures improve accessibility by reducing wait times to see a medical professional and/or reduce the physical (i.e. miles, costs) and social (i.e. education, agency) distance to health clinics.
2. Patient healthcare data collection and storage
Such projects offer technology and operational support to healthcare providers in order to improve the efficiency, navigation, accuracy and accountability of large health data sets, allowing them to gather, synthesize and store medical records. They also involve confirmation messages, health education and drug adherence reminders in addition to data collection. Due to the limitations of SMS messaging, an increasing number of initiatives use smartphone applications and/or proprietary software to collect more detailed patient information that can be easily transferred to other mobile devices or data centers.
3. Empowering medical professionals and governments
Continued and improved access to information strengthens enhanced diagnostics, disease surveillance and immunization monitoring. Such ventures help healthcare professionals to stay informed on the latest standards of care and new developments in medicine. Most mHealth endeavors rely on SMS messaging to send customers daily messages on new findings in medicine, and also provide a way for healthcare professionals to network with peers outside their area of expertise. While many projects focus on collecting data on infectious disease to strengthen decision-making during outbreaks, others focus on organization-wide data collection and storage.
4. Public education programs
Lack of health knowledge prevents individuals from seeking care. People may not understand the severity of their condition or the treatment options available to them. Thirty-two mHealth projects focused on improving health education through SMS messages, smartphone apps, Facebook pages, online videos, hotlines and online learning modules. These services provide information on childcare, affordable drugs, nutrition, diseases, sexual and reproductive health, and referrals to local care centers. The target audience for this value proposition is usually general in scope, but includes new and expectant mothers, young adults, and individuals with diseases including HIV/AIDS, hypertension and diabetes. These programs enable, motivate and educate people on adopting healthy practices and aim for long-term behavior change.
5. Payment of medical care
The rising cost of care is a barrier to health-seeking behaviors. For 21 mHealth ventures, the value proposition focused on making healthcare less expensive or easier to pay. These ventures lower costs through a combination of three approaches: 1) providing discounts or e-vouchers for medical visits via text message; 2) providing health insurance; or 3) offering low-cost medical services. Effectively, these ventures reduce net healthcare costs or offer alternative financing methods for low-income customers.
6. Adherence to drug treatment regimens
Failure to follow drug regimens poses both an individual and public health risk by increasing the odds of spreading diseases like tuberculosis. Projects aimed at improving adherence to drug regimens provide customers with text message or phone call reminders to take medication. Some ventures also provide workshops, support groups and home visits as part of their services. The primary target audience for this value proposition is pregnant women, parents of sick children (as a reminder to get children vaccinated), and individuals with HIV/AIDS, tuberculosis, diabetes and thyroid diseases. These ventures encourage the proper usage of medication, decrease the number of cases of resistant disease, and keep patients on track towards longer lives.
7. Reduction or avoidance of stigma
De-stigmatization or privacy in order to avoid stigma of diseases is important for medical care, especially for sensitive diseases such as HIV/AIDS, other sexually transmitted infections and mental illness. In such cases, knowledge of a patient’s status can affect their public perception, acceptance in the community and employment opportunities. To reduce or avoid stigma, such ventures provide confidential ways for individuals to receive information on sensitive topics, with most focusing on HIV/AIDS, contraception and family planning. Each of the ventures employs counselors or healthcare professionals to staff confidential hotlines or provide support over text messaging.
8. Increasing institutional efficiency
Inefficiencies in healthcare systems are often caused by lack of qualified employees, shortages of necessary medicines and equipment and poor resource management. This value proposition focuses on improving the efficiency of healthcare institutions by better resource management, faster diagnostics and accurate forecasting of supply inventory. Some initiatives rely on SMS messaging and paperless systems to get test results to patients in less time, while others use proprietary software to monitor supply stock, online orders, customer flow and retention and/or patient scheduling. The overall goal of such ventures is to improve the effectiveness of the existing healthcare system.
9. Quality control of care
Although it is the least common value proposition, monitoring quality of care is important for patient safety and healthcare efficiency. Each of the seven mHealth ventures that focus on quality control of care examine and authenticate the safety of medication in locations where unreliable electricity prevents proper refrigeration and can decrease shelf life. For example, by using unique identifier safety codes or through consumer reports, these ventures may indicate if a refrigerated medicine is safe or a drug is authentic. Through active feedback systems, these ventures improve quality of care by building consumer trust and accountability in their healthcare providers.
Self-Sustaining mHealth Ventures
The ultimate measure of a venture’s success is its ability to sustain itself without donations or government support. Of the 234 mHealth initiatives we studied, 42 were funded by their own revenues. Due to increasing regulation, a lack of institutional capacity to devise effective quality control regimens and the ability of institutions to pay, ventures that improve quality control of care are most likely to be sustainable. Education projects are the least likely to be revenue-funded because it is difficult to communicate the value of preventive healthcare, the knowledge offered is not directly actionable, and such organizations are seldom challenged to derive revenues from their services.
Revenue-funded mHealth ventures often minimize costs to stay competitive, offer sliding scales so people pay what they can afford, or collect client payments over a longer period of time. Such ventures tend to use simple, easy-to-maintain technologies such as phones and computers, and focus on primary care for the general population. Rather than cutting costs by cutting expertise, they employ medical professionals for extra pay alongside their formal jobs, use high-quality enabling systems and go the extra mile to deliver consistent high-quality value to their customers. Finally, they are continually striving for growth, whether in-country or expanding to other countries in hopes of serving more people. These proven practices can be adapted by new telemedicine and mHealth projects as they strive for financial sustainability.
Part one of this blog series focused on common failure modes of telemedicine and mHealth ventures and part two describes the common value propositions of such ventures. Part three will focus on how design thinking can be leveraged to build sustainable mHealth systems.
This blog is a summary of a research article: Sundin, P., Callan, J., Mehta, K., “Why do Entrepreneurial mHealth Ventures in the Developing World Fail to Scale?” Journal of Medical Engineering & Technology, Vol. 40, No. 7-8, pp 444-457, 2016)
Image credit: Andy Miah, via Flickr.
Khanjan Mehta is the Vice Provost for Creative Inquiry and director of the Mountaintop Initiative at Lehigh University.
- Categories
- Health Care, Technology