Still Waiting for a Seat at the Table: When Will Global Family Planning Focus on Smaller Private Providers?
How well is the private sector integrated into global family planning (FP) efforts? Not well enough. The current private markets trajectory in many low and low-middle income countries is not nearly sufficient, and donor-funded products and NGO programming are clearly not the entire answer.
International FP efforts are paying a heavy price for this lack of private sector involvement: Nearing 2020, the global FP community reports that despite many stellar efforts, we will fall short of the FP2020 goal of achieving 120 million new users of contraception by 2020.
I can’t go much further in this post without discussing what constitutes the private sector: Though it may seem obvious, the sector’s definition can actually be a bit slippery. Let’s start by clarifying what is not included in the private sector: It should be uncontroversial that government and donor-funded commodities and services, delivered by public and donor-sponsored, non-profit clinics and outreach teams are public sector. Conversely, we can all agree that privately-owned clinics, hospitals, retail pharmacies and drug shops operated in a for-profit model are private sector.
The slippery zone? Social marketing organizations (SMOs), which receive donor funding to design and implement education, outreach and behavior change initiatives. These SMOs procure in ultra-large quantities and deliver reproductive health services and products, often at subsidized prices and fees – and sometimes for free. SMOs have their own brands relaying quality and trust, which are often available in retail pharmacies and privately-owned clinics – so they may appear to be private sector. But sustained or non-targeted subsidies and below-market prices are not consistent with healthy market conditions, and can have unintended consequences – especially for smaller private players like clinics, retailers and wholesalers/distributors. SMOs deliver significant services to underserved markets but can also undermine these businesses, which operate without sustained subsidies, so they’re not included in my definition of private sector players.
Smaller Private Sector Players: Still Lacking a Seat at the Table
Market-based approaches are broadly accepted in family planning, as illustrated by the continued pursuit of concepts like a Total Market Approach (TMA). And there are certainly significant investments in strengthening health outcomes through the private sector (including SHOPS-Plus among others). But there needs to be an even greater focus on the private sector – and more recognition of the contributions of a wider array of private players.
The lack of a robust private sector presence on the global family planning stage was evident at the 2018 International Conference on Family Planning (ICFP), which I attended in Kigali, Rwanda late last year, and which serves as a bellwether of sorts for the global FP sector. Were private sector stakeholders invited to the table at the event? Yes and no. It’s not that they were not welcome: In the bustling Kigali Convention Center, there was certainly a good presence from large manufacturers with household names – like Bayer, Merck and Pfizer, which were among the sponsors of the conference. These companies and their representatives had exhibit booths, sponsored open events and actively participated in session discussions.
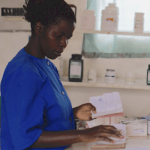
But in contrast, representation of smaller players from the private sector seemed minimal – and certainly not in proportion to their actual numbers in the FP industry. As reported by SHOPS Plus in The Private Sector: Key to Achieving Family Planning 2020 Goals, in 2016 more than 106 million women in the world’s 69 poorest countries relied on the private sector for their modern method of contraception – this is more than a third of all women who live in the FP2020 focus countries. Over 90 percent of these 106 million women are getting their contraceptives from private clinics, pharmacies or drug shops – often small and mid-size enterprises.
This limited visibility differed from other stakeholders: Faith leaders were there. So were policy makers and parliamentarians, civil society and advocacy organizations, academic researchers, dozens of NGOs, and other implementing organizations. But though some for-profit providers were among them, I didn’t notice any sessions in the massive ICFP program highlighting what smaller providers observe in their clients, and the unique challenges they face. Instead, panel presentations and posters focused much more on topics such as advocacy, in-country program design and outcomes, user needs and preferences, method adoption and adherence.
Amongst the very few ICFP sessions focused on the private sector were excellent presentations on topics such as women’s decision-making regarding where to access FP services and why (and how this might guide resource allocation), the implications of FP inclusion in health insurance for both users and providers, and the possibilities held by shifting market share from donor to commercial products for wealthier women. It was heartening to see the growing recognition that women and their partners are consumers with agency, not just for selecting FP methods but also site of care. But it would have been nice to hear more about common difficulties faced by the smaller private providers who offer that care – particularly the challenges of having to compete with free services in the public sector, and obtaining timely payments from under-financed social insurance schemes.
Why and How to Bring Smaller Players into the Family Planning Discussion
Are we being disloyal to the rights-based, social outcome approach of family planning by engaging the private sector – particularly in low-resource regions where patients’ ability to pay may be limited? No, and here’s why.
Several factors underline the family planning industry’s need for the private sector. First, the funding gap: The need for reproductive health supplies to help individuals plan their family size is not diminishing – and donor funding is projected to be insufficient, as highlighted in the recent 2018 Family Planning Market Report. Second, we know that many women prefer the private sector for reasons of access, wait time, product availability and privacy. For example, emergency contraception is a booming product in the private sector markets in several countries. Third, purchasing power is increasing, and the emerging segments of consumers with the ability and willingness to pay offer opportunities to shift market share from free and subsidized to commercial products. If we can move the top wealth quintiles – which already have FP purchasing power – towards fee-for-service approaches, that could free up limited resources to serve those in greater need.
How can the family planning sector make these changes? A greater emphasis on smaller private providers will be key. I have initiated exploratory discussions with ICFP organizing leadership as well as TMA colleagues regarding whether and how we might cultivate a more visible and formal presence from smaller private stakeholders at the conference going forward. Perhaps representation from small and mid-size private sector FP providers could be more actively cultivated? Let’s bring in private provider networks, midwife entrepreneurs, mid-size wholesalers, and other retailers trying to serve their customers and build stable businesses in their local and national communities. Let’s learn from countries that have fostered their private sectors, reaching remote communities through innovative entrepreneur models and intentional markets. Let’s go beyond the big public-private sector partnerships and think about the last mile of the provider community: What do they need in order to contribute to global FP objectives? What advocacy efforts might they welcome, and what could they contribute to a dialogue on the big stage at the ICFP, or in the more focused session rooms?
But there’s an even more important question we need to answer: How can this focus move beyond the discussion at events like the ICFP, boosting both awareness and support of the critical role private providers play across the family planning sector? It’s two years until the next ICFP, but this conversation can’t wait. Let’s get going.
Andrea Bare is a Senior Advisor with the William Davidson Institute at the University of Michigan (WDI).
Image courtesy of Dominic Chavez/The Global Financing Facility.
Homepage photo via Pexels.
- Categories
- Health Care